Prehabilitation before cancer treatment
Prehabilitation, or prehab, is an important step that helps prepare you for cancer treatment before it starts. There is evidence that even small gains in health and fitness made through prehabilitiation improves your health during treatment and recovery, even if you only get started a few days or weeks before treatment starts.
Benefits of preparing for treatment like surgery, chemotherapy or radiation therapy include:
- Feeling more in control of your mental and physical wellbeing
- Leaving hospital sooner after surgery
- Coping better with, and having fewer side effects from treatment
- Improving long-term health
Steps to prehabilitiation include:
- Diet; what you are eating and your weight
- Physical activity and exercise
- Mental and emotional wellbeing
- Stop (reduce) smoking and reduce alcohol intake.
Exercise
Staying active before treatment can have real benefits to how you manage an anaesthetic and other treatment. This may mean keeping up with your usual walks or exercise routine. For those who don't take regular exercise, introducing just 30 minutes a day of walking has proven benefits, even if you are only a few days or a week out from starting treatment.
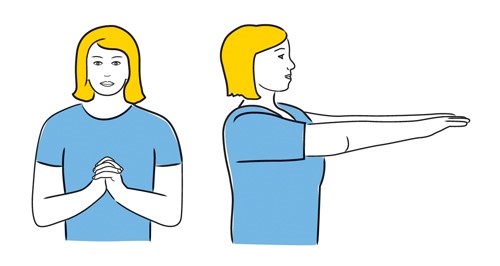
An important part of recovery from breast cancer will be the exercises you are asked to do post-operatively. Your treatment team tell you know what these exercises are and will give you written information to remind you what to do.
The exercise guide below is a good summary of the exercises you will be asked to do. Have a closer look as it is good to practice these before surgery. If you are unsure about the advice from your treatment team, make sure to check in with your breast care nurse.
Diet:
Making small, simple changes to what you eat before you start cancer treatment will make a difference to how you feel and improve recovery after treatment.
These changes include:
- Reaching out to family and friends for meals
- Preparing some meals that you can freeze
- Increasing the amount of fresh vegetables and fruits in your diet
- Limiting “fast foods”, red and processed meat, processed foods, sugar-sweetened drinks, and alcohol
- Eating the rainbow. Look for nutrients from all different types and colours of whole foods. Aim to eat at least five different colours of fruits and vegetables each day.
Emotional wellbeing
When you are told you have breast cancer it is not unusual to experience a range of emotions. This can include distress, shock, anger, fear, grief and anxiety as well as a sense of loss or feeling overwhelmed. These are natural responses to challenging situations infused with danger and uncertainty.
These emotions may be triggered at different stages of your treatment from finding a lump or being told you have breast cancer, waiting for treatments or investigations, coping with side effects of treatments, to changes in your relationships, career, finances, fertility, body image and living with uncertainty.
It is also common for those close to you to experience a similar range of emotions as they support you through your treatments.
The good news is there are many tools and resources available to help you and your whānau manage emotions at this time. You can talk these through with one of our BCFNZ nurses or take a look at the Healthify website, which provides information on managing stress.
Stop Smoking
Stopping smoking, even for a short time before treatment starts, can be one of the most important things you can do for your health and to improve the outcome of your cancer treatment. People who stop smoking experience fewer and less serious side effects from surgery, chemotherapy and radiation and also recover quicker when treatment is finished.
It can be hard to stop smoking when you feel anxious about your diagnosis. There are people and services who can help by quickly supplying the nicotine replacement therapy that is best for you and by providing ongoing practical support. Call your GP or our BCFNZ specialist breast nurses to get started on 0800 226 8773.
BCFNZ nurses are also able to advise you about vaping, so that you can make an informed decision about the type of vape you use or to stop vaping altogether.
For information and support to stop smoking, take a look at the Quitline website.
Reduce Alcohol
Stopping or reducing alcohol intake before chemotherapy or surgery starts is also important. Alcohol can interfere with the way some medications and anaesthetics work, and increases the likelihood of experiencing side effects and complications following surgery or chemotherapy. Even if you only have a short time (days or weeks) between diagnosis and treatment you will feel benefits to your health from reducing or stopping your alcohol intake. At a minimum you should not drink at least 48 hours before surgery.
More information about safe alcohol levels and support to reduce drinking is available on Alcohol.org.nz.
Need more advice?
More ideas about how to improve fitness, nutrition and emotional well-being can be found on the Keeping Fit And Well During Treatment page.
Get started
When you're ready to begin your rehab journey, fill out this form and one of our specialist breast nurses will be in touch to help.
If you have any questions or need to talk things through with someone, get in touch with our specialist breast nurses. Call 0800 226 8773 or email breastnurse@bcf.org.nz
